Fall can be a beautiful time of year. Unfortunately, it can also bring on seasonal allergies.
Allergies are your body’s reaction to a foreign substance it views as harmful, a type of “invader”, and for many people fall pollens can be big offenders. Over 24 million Americans suffer from seasonal allergies. Symptoms of these allergies can include nasal stuffiness, sneezing, runny and itchy nose, itchy throat and eyes, headaches, fatigue, sore throat, wheezing, coughing, and trouble breathing. In other words, these symptoms can make you feel downright miserable.
Common seasonal allergens
Many people are familiar with springtime allergies. The plants that are blooming which tend to most problematic are:
- Grasses – These are among the biggest offenders. You’ll need to be aware of which grasses grow in your area. If you move to another location check to see if there’s a different grass that may be a problem for you.
- Flowers – The spring flowers that are most likely to cause an issue are chamomile, chrysanthemums, daisies, and goldenrod, lilacs, and roses. But be aware that any plant pollen can be a trigger.
- Trees – Because trees are so big they tend to put out a lot of pollen, making anyone with an allergy truly miserable during this time. Just as with flowers, any tree pollen can be a candidate for inducing allergies. The most common tree allergies are to ash, birch, cedar, cypress, hickory, pine, poplar, and willow.
- Mold – Unfortunately mold can be both indoors and outdoors. And in the spring, especially in damp climates, it can cause high production of spores. Be sure to use a dehumidifier and try to keep your home as dry as possible.
But allergies don’t only happen in the spring. Common fall allergens include ragweed, sagebrush, pigweed, tumbleweed, Russian thistle, cocklebur, burning bush, lamb’s quarters, and mugwort.
Reducing your allergy exposure
Avoiding these allergens is best but really not always possible so let’s look at some ways to mitigate some of the symptoms that accompany seasonal allergies.
- Check local pollen counts
- Keep windows and doors shut on high pollen days
- Keep the windows of your car shut on high pollen days
- Use HEPA filters
- If you have air conditioning, use it on high pollen days
- Take shoes off in the house
- Vacuum daily to remove dust and pollen
- Change your clothes after working or playing outdoors
- Shower and wash your hair before going to bed to remove pollen from skin and hair
- Change your pillowcases at least a couple of times a week
- Wear sunglasses and a hat to protect your eyes from pollen
- Drink more liquids to stay hydrated which can help thin mucus in the nasal passage.
Dietary support for allergies
Your overall health can have an impact on how your body reacts to these allergens so eating a healthy diet of fresh fruits and vegetables along with quality protein and healthy fats is very important. There are various foods and herbs that can also help.
- Quercetin is believed to stabilize the release of histamines, inhibits inflammation, and helps control allergy symptoms. It is naturally found in broccoli, cauliflower, green tea, and citrus fruits.
- Nettle is a strong herb that is known as one of the best anti-allergy herbs as it is an antihistamine. It has been shown to have positive effects in the management of allergic rhinitis.
- Rosemary has antiseptic properties that can help fight respiratory infections and clear congestion.
- Garlic is considered a great natural decongestant to help relieve sinus pressure. It is the allicin in crushed garlic that helps thin mucus and reduce inflammation. It can shorten the duration of the reaction by stimulating the immune system.
- Butterbur is well researched and promising for treating seasonal allergies. It can work as well as pharmaceutical antihistamines without the drowsiness.
- Turmeric has antihistamine properties because of the active ingredient curcumin. Scientists consider turmeric to be effective in relieving the airways, combat allergic reactions by palliating the immune response. It can inhibit histamine release also.
- Ginger can help reduce inflammatory issues such as swelling and irritation in the nasal passages, eyes, and throat thereby reducing allergy symptoms naturally.
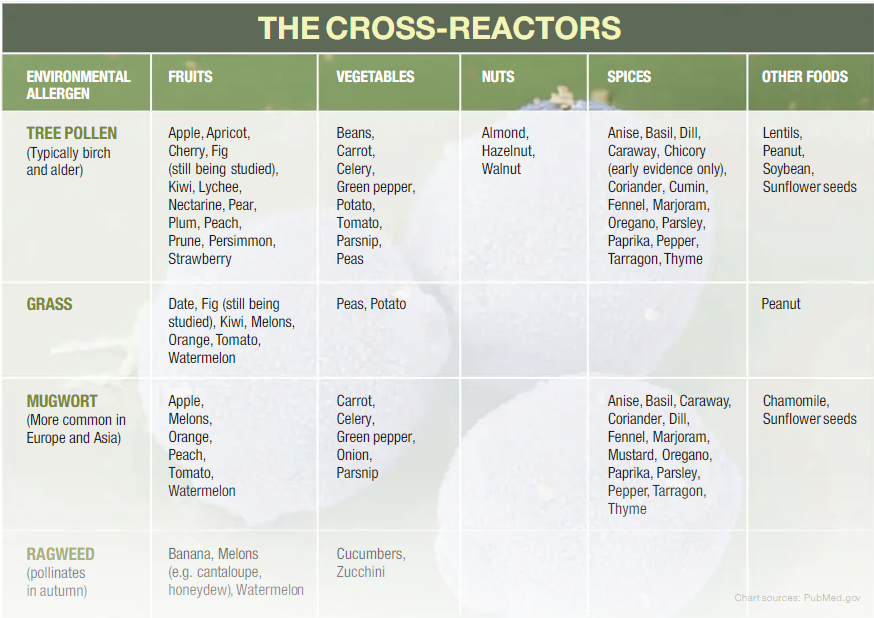
Some people who deal with seasonal allergies may also be allergic to certain foods as a result of eating allergy-triggering substances. Check out the posts about Oral Allergy Syndrome and Food Allergies
Sources
- Bakhshaee, M, Mohammad Pour AH, Esmaeili M, Jabbari Azad F, Alipour Talesh G, Salehi M, Noorollahian Mohajer M. Efficacy of Supportive Therapy of Allergic Rhinitis by Stinging Nettle (Urtica dioica)root extract: a Randomized, Double-Blind, Placebo- Controlled, Clinical Trial. Iran J Pharm Res. 2017 Winter;16(Suppl):112-118. PMID: 29844782; PMCID: PMC5963652.
- Kawamoto, Y., Ueno, Y., Nakahashi, E., Obayashi, M., Sugihara, K., Qiao, S., Iida, M., Kumasaka, M., Yajima, I., Goto, Y., N., Kato, M., and Takeda, N. (2016) Prevention of allergic rhinitis by ginger and the molecular basis of immunosuppression by 6-gingerol through T cell inactivation. The Journal of Nutritional Biochemistry, Volume 27, 112-122, Retrieved from https://doi.org/10.1016/j.jnutbio.2015.08.025.
- Kurup VP, Barrios CS. Immunomodulatory effects of curcumin in allergy. Mol Nutr Food Res. 2008 Sep;52(9):1031-9. doi: 10.1002/mnfr.200700293. PMID: 18398870.
- Schapowal, A. (19 January 2002). Randomized controlled trial of butterbur and cetirizine for treating season allergic rhinitis. Retrieved from https://www.bmj.com/content/324/7330/144.short.
- Thornhill, S. and Kelly, A. (2000). Natural treatment of perennial allergic rhinitis. Alternative Medicine Review. Volume 5 Number 5 2000. Retrieved from http://www.anaturalhealingcenter.com/documents/Thorne/articles/AllergicRhinitis.pdf.
- Yamada, S., Shira, M., Inaba, Y., and Takara, T. Effects of repeated oral intake of a quercetin-containing supplement on allergic reaction: a randomized, placebo-controlled, double-blind parallel-group study. European Review for Medical and Pharmacological Sciences. Retrieved from https://www.europeanreview.org/wp/wp-content/uploads/4331-4345.pdf.
- Yousef, M. Assessment of the effects of rosemary extract on mast cell-mediated allergic inflammation. Brock University. Retrieved from https://dr.library.brocku.ca/handle/10464/13676.