You wake up in the morning and you brush your teeth then wash your face with your all natural face wash. You’re in a hurry to get out the door for work but know you need to at least try to eat something, so you grab a ripe peach, or my favorite a crisp apple, to eat on the way to work. You take a few bites and then it starts, your mouth gets itchy and your tongue starts to burn. You start to think, “Was there something in my toothpaste? Maybe I got some of the facewash in my mouth? I think I would have known that.”
While there are real concerns with the products we use for our oral hygiene, there is another concern that may not have crossed your mind, pollen food syndrome, also known as PFS.
What is PFS?
PFS is an allergic response marked by severe itching of the skin of the lips and mouth that can come with swelling or tenderness in and around the mouth or lips.
PFS, also known as oral allergy syndrome, OAS, is distinct from another condition affecting the lips and mouth, burning mouth syndrome, or BMS.
The difference between the two conditions is the cause of the itching and burning. In BMS, the symptoms can be caused by a variety of things such as a systemic issue like diabetic nerve damage, nutritional deficiencies, hormonal changes, psychological disorders or from other causes like chemotherapy, neurodegenerative diseases like Parkinson’s, simple mouth infections like cold sores, or a candida infection.
When the condition is BMS the issue can sometimes be resolved by removal of the causative factor, such as changing to a different brand of toothpaste if the is caused by a specific chemical in it, such as sodium lauryl sulfate. In the case of systemic causes, dietary changes and treating any nutritional deficiencies can help to solve the overarching issue. In PFS the cause is from an antibody cross-reaction with proteins in the problem food.
For our immune system to work properly, a protein on a bacteria needs to be recognized by our immune system. Once recognized, our immune system can then identify and go to work attacking the problem organism. The issue in PFS, like all allergies, comes when your body starts to recognize proteins as problematic when it shouldn’t.
Fortunately, unlike other food allergies, PFS is rarely life-threatening, though this fact won’t comfort someone who suffers from PFS. A diagnosis of PFS is typically done on a case by case basis and those with PFS often have a history of hay fever with skin tests to the pollens or foods in question.
Due to the need to rule out other causative factors, people typically don’t get diagnosed until they have a medical history documenting issue. This explains why children are often undiagnosed. Some doctors will look at total or specific IgE antibodies to try and confirm an immune response and to rule out other factors.
How is PFS different?
While the itching, pain, and discomfort from PFS may seem like BMS, there are important differences. One of these differences is that those who suffer from PFS often have an allergy to something else such as a classic food allergy, or an allergy to pollen.
Another factor is that in people with PFS, the trigger foods typically come when raw food is consumed, and sufferers don’t have the same reaction when the food is cooked. If you reacted to a raw apple or peach, you typically don’t get the same reaction to a cooked fruit dessert such as an apple or peach pie. This is because the proteins that cause the reaction in the food are not heat tolerant. When these foods are cooked, the proteins will start to break down and thus won’t result in an immune response because our body is no longer able to recognize these proteins it thinks are harmful.
PFS is often seen in people who have cross-reactions to birch, grass, or ragweed pollens. People who are sensitized to birch pollen often cross-react with apple, pears, carrots, or celery and those sensitized with grass pollen will often cross-react with celery and carrots. There is concern that pesticides applied to plants may increase the expression of cross-reactive proteins in plants. This means that eating clean foods and minimizing the chemicals in our environment can go a long way in terms of prevention PFS prevention.
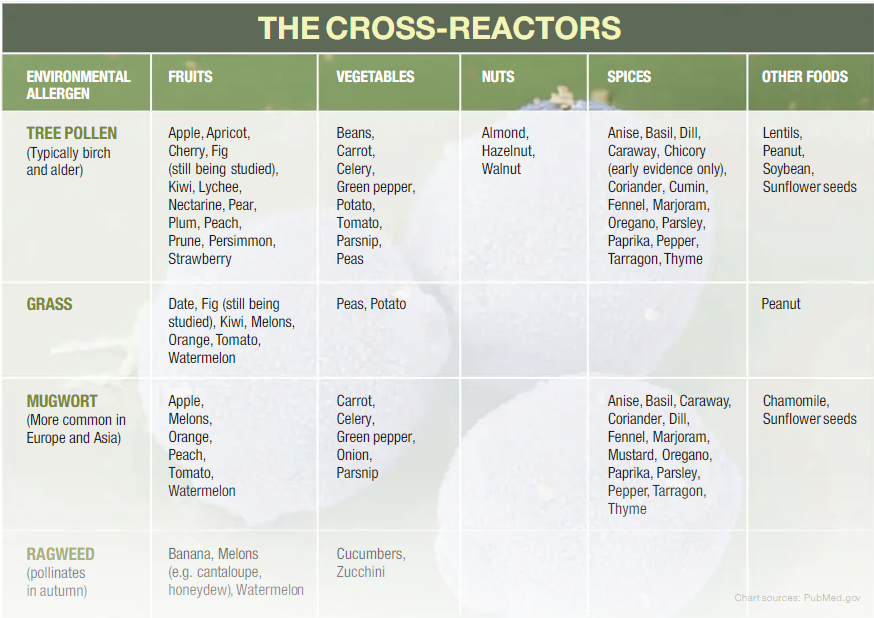
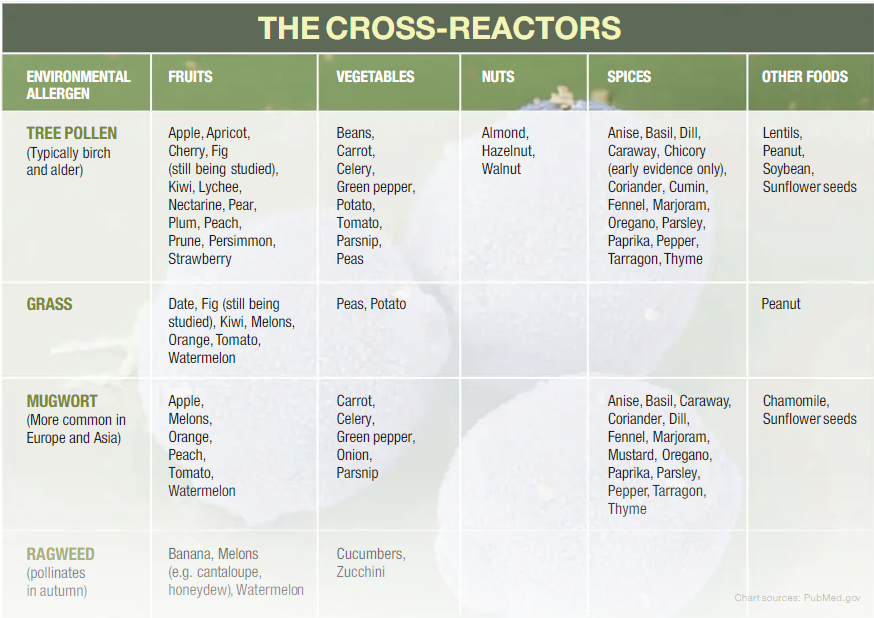
The Cross Reactors

Tree Pollen (typically birch and alder)
Fruits: Apple, apricot, cherry, fig, kiwi, lychee, nectarine, pear, plum, peach, prune, persimmon, strawberry
Vegetables: Beans, carrot, celery, green pepper, potato, parsnip, peas
Nuts: Almond, hazelnut, walnut
Spices: Anise, basil, dill, caraway, chicory, coriander, cumin, fennel, marjoram, oregano, parsley, paprika, pepper, tarragon, thyme
Other foods: Lentils, peanut, soybean, sunflower seeds
Grass
Fruits: Date, fig, kiwi, melons, orange, tomato, watermelon
Vegetables: Peas, potato
Other foods: Peanut
Mugwort (More common in Europe and Asia)
Fruits: Apple, melons, orange, peach, tomato, watermelon
Vegetables: Carrot, celery, green pepper, onion, parsnip
Other foods: Chamomile, sunflower seeds
Ragweed (pollinates in autumn)
Fruits: Banana, melons (e.g. cantaloupe, honeydew), watermelons
Vegetables: Cucumbers, zuchhini
At a glance
What to do if you have PFS?
If you suspect you have, or have been diagnosed with, PFS one of the first things you may be told is that there is no treatment available and to simply avoid the food that is causing the reaction.
As mentioned above, cooked foods don’t result in the same reaction most of the time. When the food is from a fruit like an apple, you can also remove the skin as a way to weaken or remove the reaction. The reason removing the skin works for some foods is because the skin often contains more protein than the rest of the food.
When you remove the skin, you also take the problem causing proteins with it. This should be done with caution though because fruits and vegetables can contain different amounts of the problematic protein depending on the conditions the food was grown in or how ripe it is. This means that removing the skin of one type of apple might not work while it may for another.
It’s been estimated that 47-70% of people who suffer from allergic rhinitis also have PFS. So if you have seasonal allergies it may be worth finding out if you have minor PFS symptoms that have gone unnoticed.
[expand title="Sources"]
Allergic Living. (2010). Oral Allergy: Plants, Foods That Cross-React. Retrieved from: https://allergicliving.com/2010/08/30/the-cross-reactors/
Coculescu, E. C., Ţovaru, Ş., & Coculescu, B. I. (2014). Epidemiological and etiological aspects of burning mouth syndrome. Journal of Medicine & Life, 7(3), 305-309Hofmann, A., & Burks, A. W. (2008). Pollen food syndrome: update on the allergens. Current Allergy and Asthma Reports, 8(5), 413-417.
Ludman, S., et al. (2016). Pollen food syndrome amongst children with seasonal allergic rhinitis attending allergy clinic. Pediatric Allergy & Immunology, 27(2), 134-140. doi:10.1111/pai.12504
Ivković-Jureković, I. (2015). Oral allergy syndrome in children. International Dental Journal, 65(3), 164-168. doi:10.1111/idj.12164
Portnoy, J. (2015). IgE in clinical allergy and allergy diagnosis. World Allergy Organization. Retrieved from: http://www.worldallergy.org/professional/allergic_diseases_center/ige/
Rivinius, C. (2009). Burning mouth syndrome: Identification, diagnosis, and treatment. Journal of The American Academy of Nurse Practitioners, 21(8), 423-429. doi:10.1111/j.1745-7599.2009.00424.x
Seto, C. (2010) OAS- When raw food is forbidden. Allergic Living. Retrieved from: https://allergicliving.com/2010/07/02/oral-allergy-syndrome-a-life-without-fruit/
[/expand]